sleep disorders
OK, should I take melatonin or not?
December 10, 2013
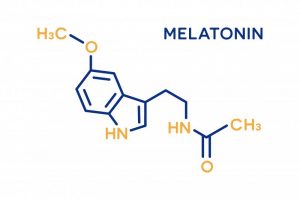
I would like to say that I have a definitive answer for that question, but as it turns out, the answer is: “It depends”. There is a plethora of research out there on the effects of melatonin, and most studies show it to have benefits even beyond helping you sleep. However, I will keep my comments related to sleep, as this is the reason most of you are taking (or have taken) melatonin.
(more…)Correspond with sleep physicians
September 12, 2013

Q: I know that quite a few board certified sleep physicians send you patients who are CPAP non-compliant or don’t qualify for CPAP. How did you gain their trust? I can’t find any in my area who will send me these patients!
Dr. Smith: I send letters after seeing every sleep patient to the MD who diagnosed the sleep apnea, detailing everything I checked, my findings, treatment attempts, etc.. . If there is one common complaint I heard from the sleep physicians at Sleep 2009 in Seattle, it’s the fact dentists do not follow up with the sleep physician after they receive the patient. That is so sad, after the grief we give them for not involving dentists. If you are a dentist reading this, PLEASE keep the sleep physician in the loop!
How Does Exercise Affect Your Sleep?
August 29, 2013

Working out especially cardio improves the length and quality of your sleep. Yes, getting sweaty during the day can help your slumber that evening….just be sure to take a bath or shower before crawling under the covers!
(more…)Pilots And Sleep Apnea
July 18, 2013
Question:
I know somebody who is a pilot. They can not be diagnosed with sleep or it is immediate disability and they can’t pilot the plane. MY question is have you ever done the MAD for this type of person without the diagnosis? What would the liability be if you said it was just for snoring?
Dr. Smith:
This is one reason we have ambulatory (home) monitors, so we can rule out anything more severe. I would insist on at least this, and you can keep it away from insurance and any official diagnosis. The liability would be pretty heavy if he fell asleep at the controls, thinking he was cured, when in fact you had created a “silent apneic”, so you really need to get at least a Level 4 study done on this patient.
Anti-depressants & Sleep Studies
June 27, 2013
Question:
I have a patient who has opted to seek counsel with their physician regarding a sleep study. She has tremendous daytime drowsiness among other symptoms.
Originally, her doctor persuaded her to not visit a sleep center for reasons I can only imagine. In the meanwhile, at my prodding, she has visited her doctor again and he wrote a script for a PSG study at her local hospital. However, the doctor also prescribed Lexapro to ‘keep her alert’ during the day so that she would have a nice sleep the nite of the study. If I remember from your class, that class of drugs limits or reduces REM sleep. Do I recall correctly?
Dr. Smith:
Lexapro and other anti-depressants will remove REM sleep, which indirectly improves the AHI, but at the expense of a valuable segment of sleep. They will sleep better if their anxieties are preventing sleep initiation, so it can be helpful, but will not give a true picture of the patient’s sleep architecture. That may or may not matter to the sleep physician, but I would ask the expert before deferring to the general MD.
Screening For Sleep Apnea
June 20, 2013
Question:
I seem to have a couple of patients who complain of snoring and want me to make them a snoring appliance, but are reluctant to spend the time & effort to go to the sleep clinic for a baseline.
How would you feel about screening these patients with a home monitor to r/o significant apnea? If the screening is negative, I would go ahead and make the snoring appliance with some degree of confidence that I was not ignoring an apnea problem. If it is positive, then use the results of the screening to encourage them towards complete diagnosis for sleep apnea.
What monitor would you suggest for this? Also, would I need to be certified to read the results?
Dr. Smith:
That’s an OK plan, as long as you follow them up with home monitoring to make sure the appliance is removing any events. That way, you can treat anyone up to about 30 events per hour, and even higher numbers if they have failed CPAP. There is no certification for reading the studies, but it does take some education. I love the Watch-PAT 200, but it’s more robust, and you may want to spend less. The ApneaLink is a “screener” at a lesser fee, but it all depends on what you want.
In great shape, but sleep apnea exists?
June 6, 2013

Q: I don’t get it, thought in order to have sleep apnea you had to be old, over weight and ugly, not in that order… I went to the Doc about restless leg syndrome and she said we need to do a sleep study and see just how bad you got it. Well I got it worst than I thought. I walked in to the waiting room at 8:45 pm and 5 other guys were sitting there cracking jokes about how their wife’s don’t put out any more and waiting to be escorted back to our rooms.
(more…)Surrounded By Snorers
May 30, 2013

Q: What is it with men and snoring??!! I don’t know many men who can honestly say that they don’t snore. My father-in-law did it; my dad does it. And, now, I am double-whammied, because I have not only one man in my house who snores but two!
(more…)